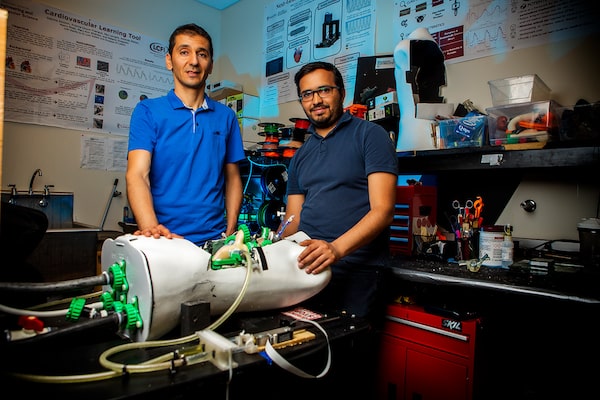
Lyes Kadem, professor and curriculum director of Concordia’s Department of Mechanical, Industrial and Aerospace Engineering (left) and Ahmed Darwish, Co-Director of Laboratory of Cardiovascular Fluid Dynamics, with heart simulator. Cardiologists and their patients who have received mechanical heart valve replacements will benefit from Concordia-led research.SUPPLIED
At Concordia University, “Next-Gen Research” is the driving philosophy behind an interdisciplinay approach which combines learning opportunities with wider social trends – a problem-solving mandate that equips today’s students for tomorrow’s fast-changing world.
The university’s cutting-edge labs and a rich cross-fertilization of ideas and expertise facilitate the development of transformative technologies that will benefit Canadians for generations to come. In the health-care field, they will lead to improved patient outcomes with less invasive surgeries and faster recoveries.
Lyes Kadem, professor and curriculum director in the Department of Mechanical, Industrial and Aerospace Engineering, illustrates this ethos. His ground-breaking research in the area of cardiovascular flow has the potential to create a major shift in the practice of cardiac medicine.
“In our laboratory we try to bridge [the space between] engineering and medicine,” says Kadem, who is also the Concordia University Research Chair in Cardiovascular Engineering and Medical Devices. “Engineers see the body as a complex machine that has to follow the laws of physics. We can learn from it and improve it.”
Dr. Kadem describes transformative technology as “a paradigm shift: something that will change the way we are doing things, the way we look at things.” His goal is two-fold: to design and test advanced cardiovascular medical devices and to improve the training possibilities of the medical practitioners who will use them.
Transformative technology is a paradigm shift: something that will change the way we are doing things, the way we look at things’
— Lyes Kadem, Professor, Department of Mechanical, Industrial and Aerospace Engineering, Concordia University
Under his supervision, Dr. Kadem’s engineering students have created a functioning heart simulator – made of pipes and motors, pushers and pullers, “soft” robotics and “origami” robots – that replicates the flow of blood through the cardiovascular system. A 3-D printed clone of a real heart can then be put into the machine and start to beat.
“This is not trivial,” he says. “It lets us perform measurements under repeatable and controlled conditions.”
Personalized medicine
Dr. Kadem’s system will allow designers to move away from “one-size-fits-all” devices: Prosthetic heart valves, for example, are currently produced in standard sizes which may not be an exact fit for every patient. A CT scan can be made of a sick patient’s heart; it is 3-D printed and then placed in the simulator. The data produced will make it possible to create a custom-made device that fits perfectly, designed with the patient’s specific pathology in mind. “Personalized solutions are the future of medicine,” he says.
Current devices are tested on healthy animals – usually pigs – and therefore do not truly reflect the disease model. “It’s like testing winter tires in summer,” he says. “This means that the patient is carrying all the risk.” The simulator will allow a prospective device to be tested on a portfolio of many different patient models before being approved for general use.
Dr. Kadem’s research does not stop at the laboratory. He is also currently engaged in a collaborative project with Dr. Brian Potter, an interventional cardiologist at the University of Montreal Health Centre, whose work in the ICU involves the sickest cardiac patients, those in the throes of heart failure.
“We’re trying to develop a simulator that will be useful in the area of cardiogenic shock,” Dr. Potter explains. “When the heart pump fails, the blood can’t circulate strongly enough, so there’s a lot of interest in temporary artificial heart pumps.”
Dr. Potter’s team has succeeded in developing a cardiogenic shock model on a pig. The resulting data, fed into Dr. Kadem’s simulator, will allow future artificial pumps to be accurately tested, without the need for animal experimentation.
The study is expected to come to fruition this summer. “Simulation is clearly a key component of future heart research,” notes Dr. Potter. “We can get new data that was never available before.”
He envisages future projects with Dr. Kadem: “It’s been quite fertile. There’s only so much you can do in siloed research; collaboration generates that creative spark that leads to true innovation.”

Dr. Marta Kersten-Oertel, assistant professor in the Department of Computer Science and Software Engineering: “We are working on developing the next generation of tools to be used in operating rooms.”Christinne Muschi
AR technology
In a completely different field, it is this same creative spark that drives the research of Dr. Marta Kersten-Oertel – assistant professor in the Department of Computer Science and Software Engineering and Concordia University Research Chair in Applied Perception– as she harnesses the augmented-reality technologies of the computer-gaming industry to develop software tools that could transform the practice of neurosurgery.
“We’re developing methods to enhance the perception of medical images, using this new generation of technology in image-guided neurosurgery,” she says.
In conventional neurosurgery, CT or MRI images are displayed on a monitor in the operating room. Her lab’s technology merges an accurate three-dimensional map of the patient anatomy and diseased area directly onto the patient’s skull, allowing the surgeon to work with greater precision.
“Instead of looking away at a screen, they can get all the guidance information they need, right in their field of vision,” she explains. “We’re working on figuring out which visualizations are best to most accurately and safely guide the surgeon.”
Sound for surgery
Dr. Kersten-Oertel is also experimenting with the use of sound to guide surgeons’ tools to a desired target, much like the beeping of a car’s backing-up system. “Taking advantage of sound allows surgeons to reduce their dependency on visual information, thereby increasing available attention for other tasks,” she says. “This is something quite new. We are working on developing the next generation of tools to be used in operating rooms, to help surgeons and ultimately improve patient outcomes.”
She considers Concordia’s interdisciplinary approach to be essential to her research. “There are good possibilities for collaboration and strong engagement with the community,” she says.
“We are able to showcase the lab’s research, which has generated a lot of interest,” she continues. “Interaction with the community is vital when developing technologies that have the potential to impact society.
Advertising feature produced by Globe Content Studio with Concordia University. The Globe’s editorial department was not involved.