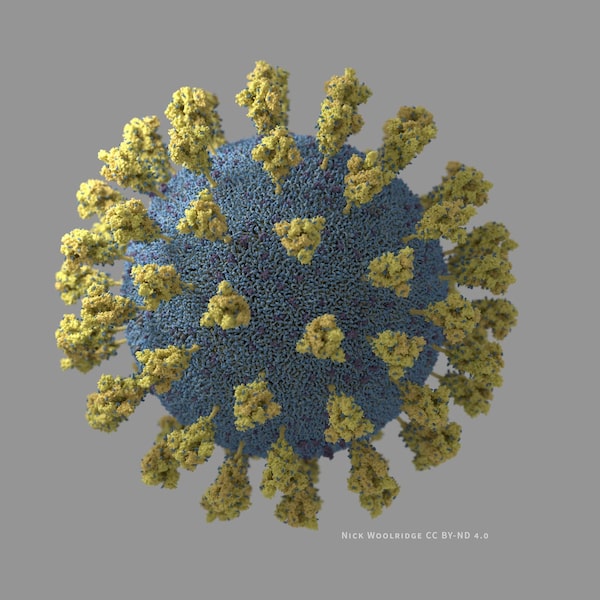
A 3D illustration of a SARS-CoV-2 virus particle.Nick Woolridge/Biomedical Communication
Anyone curious to see evolution playing out in real time need look no further than NextStrain.org, a website that depicts the ever-sprouting family trees of different pathogens residing in the human population.
Maintained by a collective of computational biologists, NextStrain is currently displaying more than 3,500 genetically distinct branches of SARS-CoV-2, the virus that causes COVID-19. Those are just a selection of all the variations that have been seen. More are showing up all the time, thanks to the immense opportunity for diversification that the virus has gained by infecting about 80 million people this year.
Mostly, these dissimilarities lead to identical behaviour in the virus. Like fingerprints, their genetic codes are useful for identification and for tracing the history of various outbreaks. But the disease they cause is the same.
That is not the case for a new variant, first spotted in Britain and now known to be in Canada. Based on epidemiology and preliminary lab reports, the variant may be shifting the character of COVID-19 enough to make a difference in how the disease spreads and who catches it.
This has caused concern not only because of the potential for the pandemic to accelerate, but because a changing virus may become harder for standard COVID-19 tests to spot and for newly approved vaccines to defend against.
The same concern extends to two other variants that have gained attention in recent days, one from South Africa and one from Nigeria. Neither is closely related to the U.K. variant but both share with it a mutation in their viral genomes that influences how the virus latches on to human cells. The mutation, known as N501Y, has been seen before, but the U.K. and South African variants in particular seem to have bundled it with other changes that may be increasing its effect. The fact that the mutation has arisen independently a few times is evidence that it is doing something that benefits the virus.
When will Canadians get COVID-19 vaccines? The federal and provincial rollout plans so far
“When you start to see parallel evolution of certain mutations that rise in frequency, then that’s a sign that there’s a real biological advantage to them,” said Jeffrey Joy, a research scientist in evolutionary genetics at the BC Centre for Excellence in HIV/AIDS.
On Saturday, Barbara Yaffe, Ontario’s Associate Chief Medical Officer, announced that a couple living in Durham Region, east of Toronto, have the U.K. variant of the virus. This marks the variant’s first known appearance in North America. The couple did not travel which means that the variant has made one or more jumps since arriving, a situation that could potentially indicate more general community spread.
Prior to the announcement, the search was already on to see if any of the new variants are present in samples from previous cases in Canada that have been gathered but whose viral genomes have yet sequenced and identified, said Gary van Domselaar, chief of bioinformatics at the National Microbiology Laboratory in Winnipeg.
The laboratory, which is part of the Public Health Agency of Canada, is heading up daily meetings of a working group that includes representatives from regional centres in Quebec, Ontario, Alberta and British Columbia where much of the sequencing of virus genomes in Canada has taken place.
Earlier this week, reporters pressed federal officials to say if enough was being done to screen for the variants. To date, Canada has sequenced about 25,000 viral genomes since the pandemic began. As a straight total, this is about one fifth of what has been done by Britain. But those involved in the Canadian effort point out that it amounts to about the same fraction of cases as Britain has sequenced, which is about five per cent.
Such numbers reveal that even if sequencing was vastly ramped up, the pandemic is too widespread to surveil in a comprehensive way with existing resources. So if Canada can only screen a fraction of its total case count for genetic variants of the virus, those doing the sequencing are faced with having to choose which fraction.
Until now that has involved dividing resources about 50-50 between watching for changes in the virus coming in from abroad versus those that might arise naturally within Canada, said Catalina Lopez-Correa, executive director of the Canadian COVID Genomics Network.
This week, the working group has been sorting out how to shift priorities to address the threat of the new variants. That will certainly include an emphasis on international travellers and their close contacts who have tested positive for COVID-19. It may also involve looking at the viral genomes from “superspreader” events that could help a new variant to gain traction after it has already arrived.
“This week has really put genomics in the spotlight,” Dr. Lopez-Correa added.
The British variant, known as B.1.1.7, raised alarm bells last weekend because it is associated with an increase in cases in the southeast of England, where it likely originated and where it has outpaced other versions of the virus. This prompted Canada to suspend incoming flights from Britain until Jan. 6. It is also another clue that evolution is shaping the trajectory of the variant.
Genetic variants can easily become ubiquitous when they spread through a population where there is no other version of the virus around, a phenomenon known as at the “founder effect.” But B.1.1.7 managed to take over in an environment with lots of coronavirus already around. That means whatever it’s doing, it’s doing it better.
This is is probably due to the large number of mutations the new variant carries – 23 in all, with 17 of them leading to physical changes in the viral proteins. Typically, the SARS-CoV-2 virus accumulates one or two genetic mutations per month.

The viral RNA packed into the core.Nick Woolridge/Biomedical Communication
“This suggests that there was a higher rate of molecular evolution in the branch of the family tree immediately before B.1.1.7,” Dr. Joy said.
Those changes would have arisen in a single individual, possibly an immune-compromised patient undergoing therapy for a prolonged bout of COVID-19. A study published earlier this month in the New England Journal of Medicine demonstrates the potential of such a scenario to repeatedly challenge the virus and favour the emergence of a rare genetic combination. Evidence is mounting that in the case of B.1.1.7, the result is higher rates of infection.
One of the mutations slightly alters the structure of the virus’s spike proteins – the protrusions that stick out of the coronavirus – at precisely the place where they can fix onto human cells. The South African and Nigerian variants also exhibit this change, called N501Y, and it has turned up elsewhere before. The change has been shown to increase transmission in laboratory studies. Other tweaks may improve the odds of the spike protein being in the right configuration when it makes contact with host cells as well as its ability to seal the deal by efficiently fusing with its target.
Marceline Côté, a molecular virologist at the University of Ottawa, said she expects to start studying some of the changes in her laboratory to determine precisely how they might be benefiting the virus. She added that the details of how the spike protein of SARS-CoV-2 behaves are notoriously complex and not entirely understood, despite initially appearing genetically similar to that of the original SARS virus.
“It has a lot of tricks up its sleeve that we didn’t necessarily expect,” Dr. Côté said.
A key question is whether the new variants alter the spike protein enough to thwart the efficacy of the first round of COVID-19 vaccines. While the question must be put to the test, Dr. Côté noted that the vaccines are made to stimulate a response to multiple parts of the spike, not just the few areas that have changed in the variants. With luck, many of the antibodies that the vaccines stimulate will still serve to lock up the virus and prevent if from infecting cells.
In a statement, vaccine-maker Moderna Inc. expressed confidence that the change would not affect the immune response to the the spike protein induced by its vaccine, approved by Health Canada on Wednesday. The company added that, “We will be performing additional tests of the vaccine in the coming weeks to confirm this expectation.”
The impact of a slight change to the spike has been observed before, most notably when a European variant of the virus took over from the one that began the pandemic. That version became dominant in Canada early in the pandemic.
According to Sandrine Moreira, a bioinformatics specialist with Quebec’s public health lab, the European variant arrived early on, before travel restrictions were imposed. During that time, “we observed huge diversity” in the genetics of the virus as infections arrived from different parts of the world. That diversity later decreased during lockdown, and Dr. Moreira said that the analysis has yet to be done for summer and fall when some international travel resumed.
“What I suspect is that we’ll see increased diversity because of new introductions,” she said.
A modelling study posted online Wednesday by researchers at the London School of Hygiene and Tropical Medicine shows why this matters. The analysis estimates that the new variant is 56 per cent more transmissible. That does not mean the disease is more severe – the study found no clear evidence on this point, either way.
But the authors note that higher transmission means more cases overall with the public-health measures that are currently in place, which means more people in hospital and more deaths because of COVID in 2021.
“It may be necessary to greatly accelerate vaccine rollout to have an appreciable impact in suppressing the resulting disease burden,” the authors point out.
Epidemiological data in Britain also indicates that the new variant may be more able to infect children. That would fit with the evidence that the new variant is more easily able to bind to human cell receptors. The change would amount to a “levelling the playing field” for infection as a function of age, said Wendy Barclay, a virologist at Imperial College London, during a Q&A session with reporters on Tuesday.
Jesse Papenburg, a pediatric infectious disease specialist at the Montreal Children’s Hospital, said the theory hangs together but he cautioned that there are many other factors that may influence why children tend to be less susceptible to COVID-19. One of those is the yet-to-be-determined impact of previous infections by other human coronaviruses.
“I think that may be one of the missing links that, with time, we’ll be able to figure out.”
In the short term, however, the U.K. variant’s arrival in Canada could prove to be a no-win situation for public health officials, particularly if children proved to be more susceptible, said Jason Kindrachuk, a medical microbiologist at the University of Manitoba. Among other measures, it puts on the table the prospect of implementing or extending school closings in order to keep the variant at bay.
Reflecting on the situation – almost as a metaphor for the entire year – Dr. Kindrachuk added, “It’s frustrating, it’s complex, it’s intriguing … and we’re trying to temper all of that in some fashion to be able to learn what the hell is going on.”
Sign up for the Coronavirus Update newsletter to read the day’s essential coronavirus news, features and explainers written by Globe reporters.
 Ivan Semeniuk
Ivan Semeniuk