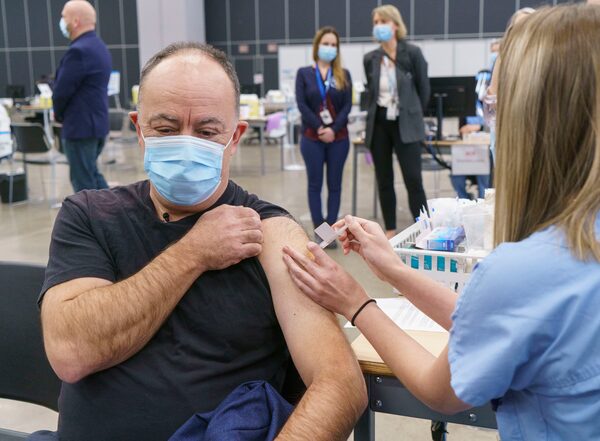
Quebec Health Minister Christian Dube receives the AstraZeneca vaccine at a COVID-19 vaccination clinic in Montreal on March 18, 2021.Paul Chiasson/The Canadian Press
Since Canada’s COVID-19 vaccination campaign began, Quebec has sometimes set aside Ottawa’s advice to forge its own path, decisions first criticized as experiments that later became mainstream.
How Quebec carved an independent vaccination plan comes from the province’s distinct public health history and autonomous political culture, relying on its own long-standing expertise and looking beyond Canada’s borders to evaluate the latest evidence.
“Quebec is very jealous of protecting its capacity to influence and regulate anything that has to do with vivre ensemble [social harmony] and culture, which writ large includes community health,” said Louise Potvin, a professor of public health at the University of Montreal. “They have a lot of expertise and research capacity, which gives them more independence. This matters a lot when you perceive yourself as a distinct society.”
Tracking Canada’s COVID-19 vaccine rollout plans: A continuing guide
Canada pre-purchased millions of doses of seven different vaccine types, and Health Canada has approved four so far for the various provincial and territorial rollouts. All the drugs are fully effective in preventing serious illness and death, though some may do more than others to stop any symptomatic illness at all (which is where the efficacy rates cited below come in).
- Also known as: Comirnaty
- Approved on: Dec. 9, 2020
- Efficacy rate: 95 per cent with both doses in patients 16 and older, and 100 per cent in 12- to 15-year-olds
- Traits: Must be stored at -70 C, requiring specialized ultracold freezers. It is a new type of mRNA-based vaccine that gives the body a sample of the virus’s DNA to teach immune systems how to fight it. Health Canada has authorized it for use in people as young as 12.
- Also known as: SpikeVax
- Approved on: Dec. 23, 2020
- Efficacy rate: 94 per cent with both doses in patients 18 and older, and 100 per cent in 12- to 17-year-olds
- Traits: Like Pfizer’s vaccine, this one is mRNA-based, but it can be stored at -20 C. It’s approved for use in Canada for ages 12 and up.
- Also known as: Vaxzevria
- Approved on: Feb. 26, 2021
- Efficacy rate: 62 per cent two weeks after the second dose
- Traits: This comes in two versions approved for Canadian use, the kind made in Europe and the same drug made by a different process in India (where it is called Covishield). The National Advisory Committee on Immunization’s latest guidance is that its okay for people 30 and older to get it if they can’t or don’t want to wait for an mRNA vaccine, but to guard against the risk of a rare blood-clotting disorder, all provinces have stopped giving first doses of AstraZeneca.
- Also known as: Janssen
- Approved on: March 5, 2021
- Efficacy rate: 66 per cent two weeks after the single dose
- Traits: Unlike the other vaccines, this one comes in a single injection. NACI says it should be offered to Canadians 30 and older, but Health Canada paused distribution of the drug for now as it investigates inspection concerns at a Maryland facility where the active ingredient was made.
How many vaccine doses do I get?
All vaccines except Johnson & Johnson’s require two doses, though even for double-dose drugs, research suggests the first shots may give fairly strong protection. This has led health agencies to focus on getting first shots to as many people as possible, then delaying boosters by up to four months. To see how many doses your province or territory has administered so far, check our vaccine tracker for the latest numbers.
The province made two decisions some considered risky – delaying second doses and giving the AstraZeneca vaccine to older people – that eventually gained widespread acceptance. The machinery behind those decisions dates back decades.
In 1998 in the wake of the second failed independence referendum, the Parti Québécois government created Canada’s first provincial or federal public health research institute. The Institut national de santé publique du Québec (INSPQ) became a quasi-independent expert advisory body that has led research on everything from how to handle heatwaves in Montreal to cutting the smoking rate in half in Quebec over the past 20 years.
The INSPQ became the umbrella organization for provincial laboratories and advisory bodies such as the Quebec immunization committee, which for 30 years has told the province the best way to deliver shots. The INSPQ studies the efficacy of those and other public health decisions.
“I think it’s good to have the capacity to adapt to the reality in Quebec,” said Nicholas Brousseau, the chair of the Quebec immunization committee and a specialist in biological risk and workplace health at the INSPQ. “We are able to examine issues like frequency of illness in our own backyard when we recommend a plan.”
Quebec has been the hardest-hit province since the pandemic started, with nearly half of Canada’s 22,580 deaths but less than one-quarter of the population. Quebec also has the highest proportion of vulnerable people aged 65 and over outside Atlantic Canada.
When vaccines started arriving in December, Quebec sent most of them directly to long-term care homes rather than hospitals, as many other provinces did.
On Dec. 18, the INSPQ immunization committee recommended delaying second doses until 1.7 million Quebeckers in priority groups, mostly people 70 and over, each received a first dose. The plan ignored manufacturers’ schedules and advice from the National Advisory Committee on Immunization (NACI), which said provinces should stick to the manufacturers’ plans of 21-to-28 day delays. Half of those people have now received a first dose.
A month later, the province decided to delay second doses up to 90 days. The government led by Premier François Legault and Public Health Director Horacio Arruda approved the plan. By February, reports from the INSPQ and the British Columbia Centre for Disease Control (BCCDC) said the plan was working to stop serious illness and death. Other provinces adopted the delay plan, extending it up to four months. “It was an example where Quebec was innovative and other jurisdictions followed,” Dr. Brousseau said.
Early this month, Dr. Brousseau’s group went against NACI guidelines to recommend giving the AstraZeneca vaccine to people over 65. In the clinical trial, the number of adults 65 years of age and over was too small to give a reliable estimate of how well the vaccine works in this age group, but the most recent real-world studies in Britain showed it was very effective. NACI reversed itself to follow the INSPQ recommendations March 16.
“It’s normal when the science is evolving so rapidly that different organizations can reach different conclusions,” Dr. Brousseau said “It’s healthy to have these debates.”
While health is a provincial responsibility under the Constitution, Ottawa purchases and approves vaccines and has its own public health research and advisory capacity. But the provinces still have the power to decide how to give shots.
The Public Health Agency of Canada was established in 2004 after the SARS epidemic and Ontario Public Health, which has a research division, followed in 2008. The BCCDC was part of the Vancouver health board before becoming a provincial agency.
Trevor Hancock, a retired professor of public health at the University of Victoria, pointed out provinces and cities have been in charge of public health for more than 100 years. “PHAC is the new kid on the block,” he said.
“The beauty of having 10 different health departments in the provinces is that there’s room for diversity and experiment,” Dr. Hancock said.
While Ontario and B.C. have considerable public health research capacity, “the added element of Quebec nationalism” further separates the province from the others, Dr. Hancock said.
Mr. Legault, himself a onetime separatist who now promotes Quebec autonomy within Canada, doesn’t hesitate to chart his own path with the recommendations from the INSPQ and its vaccination committee. Still, within Quebec, the vaccine decisions were controversial, as were other INSPQ recommendations that led the government to slowly adopt mask use and decide against installing air purifiers in schools.
“Whether it be wearing masks or the timing of a second dose, it is not treating people as guinea pigs to make decisions amid uncertainty, or to change course,” Dr. Hancock said. “That’s good science. Science doesn’t mean certainty.”
Editor’s note: A previous version of this story said clinical trials for the AstraZeneca COVID-19 vaccine suggested it was less effective with older people. In fact, the clinical trial lacked data on older people.
Sign up for the Coronavirus Update newsletter to read the day’s essential coronavirus news, features and explainers written by Globe reporters and editors.
 Les Perreaux
Les Perreaux