B.C. Health Minister Adrian Dix announced this week that he didn’t expect any elective surgeries in the province to be cancelled as a result of the deadly second wave of COVID-19.
This undoubtedly came as a relief to those who have been waiting months to get various ailments addressed on an operating room table. And it unquestionably made Mr. Dix pleased as well, given the remarkable job health professionals in British Columbia have done clearing up backlogs created by the suspension of surgeries last spring when the pandemic first arrived.
It’s an achievement that stands out amid the gloom the virus has brought to the world. And for Mr. Dix, the accomplishment is personal, having staked his reputation on reducing wait times and having taken a firm stand against private clinics, which justify their existence by arguing that waiting lists are too long and that people are suffering needlessly as a result. Last year, a B.C. Supreme Court judge sided with the government in its bid to close private clinics on the grounds that they violate the Canada Health Act; the case is likely to end up at the Supreme Court of Canada.
More than 30,000 surgeries were postponed over two months when the virus hit – a demoralizing development for the Health Minister. By the time surgeries resumed in late May (some emergency surgeries were still performed), there were about 93,000 people on a waiting list; at the time, it was estimated it would take two years to clear the backlog.
“It was tough for a lot of people, but obviously none more so than the people who were suffering and scared as a result of these cancellations,” Mr. Dix told me. “I took that personally. I thought about those people every day.”
He decided extraordinary action was needed to aggressively assault the waiting list once it was deemed safe enough to resume surgeries. He put Michael Marchbank, a former health care executive, in charge of creating a plan.
It started with money – an additional $250-million a year. In part, the new funding was used to hire more staff: 755 people, a group that included surgeons, nurses, physiotherapists, diagnostic imaging technicians and post-anesthesia care aides, among others. The province bought additional MRI machines and started running them 24 hours a day, seven days a week.
“We also focused on little things, like making sure the first surgery of the day starts on time,” Mr. Dix said. “It doesn’t sound like a big thing, but if you’re late right off the bat you’re in trouble the rest of the day.”
In the past, patients on waiting lists were often attached to a particular doctor rather than the first one available. That also changed, adding hundreds of hours of operating room time.
The result has been extraordinary – a true pandemic success story.
Last month, Mr. Dix announced that 90 per cent of patients whose surgeries were postponed during the first wave of COVID-19 had had their procedures completed. Mr. Marchbank said a backlog that was supposed to take two years to clear was likely going to be gone in 15 months.
As an example of the stunning pace at which surgeries have been taking place, Mr. Dix said that over Christmas there were 250 more surgeries performed than over the same period in 2019.
“When you think about that, it’s truly remarkable amid a pandemic,” Mr. Dix said. “Every surgery takes longer because of the safety precautions you need to put in place because of the virus, so that’s an added challenge. It just makes what our doctors and nurses and operating room teams have done – and they’re the real heroes here, make no mistake – all the more extraordinary.”
Of course, the logical question that stems from all this: Why did it take a pandemic before we saw this level of resolve in tackling unacceptable waiting lists? And will that drive continue after the virus is gone?
Mr. Dix is hopeful the new protocols will help reduce waiting lists in the future. The pandemic forced health administrators to search for efficiencies where they hadn’t searched before. It also took hiring hundreds of more health professionals to do the job.
“Look, wait lists are always going to be an issue to some degree,” Mr. Dix said. “But I think we have found some ways to make them less of a problem in the future. Fingers crossed.”
Keep your Opinions sharp and informed. Get the Opinion newsletter. Sign up today.
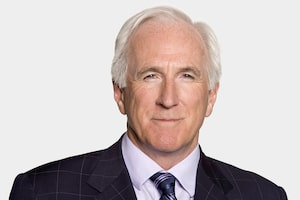 Gary Mason
Gary Mason